A recent animal study by cancer researchers at Washington State University led to a discovery related to a specific type of white blood cell. The researchers believe their findings could be used to improve the effectiveness of cancer immunotherapy in patients with melanoma and breast cancer tumors, and possibly other types of cancer. Let’s take a closer look at this discovery and what it may mean for the future of cancer immunotherapy.
The current state of cancer treatment
Immunotherapy is a relatively new approach to cancer treatment. A wealth of research has been conducted on various forms of immunotherapy and several are currently available to patients, but scientists still have much to learn about this treatment and how it can be used most effectively.
The main approach to cancer treatment still involves chemotherapy, radiation therapy, and surgery, depending on the circumstances of the disease. Like immunotherapy, these treatments also face several significant hurdles. Many cancers are unresponsive to these treatments, especially those that spread from the main tumor to the rest of the body. Additionally, some cancer stem cells develop resistance to chemotherapy and radiation.
Challenges in cancer immunotherapy
Many types of cancer immunotherapy have shown promise, but relatively few cancer patients respond to the currently available options. This low response rate is one of the most significant hurdles that immunotherapy researchers need to overcome in order to maximize the potential of these exciting new treatments.
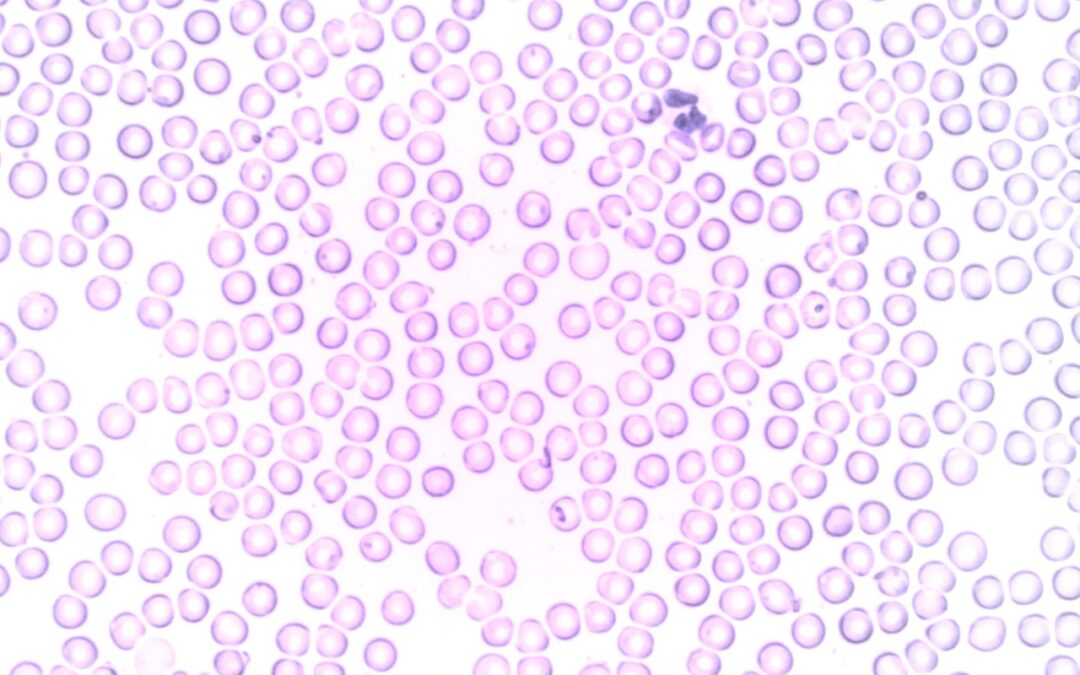
Researchers have been working to better understand the process of lymphocyte infiltration into the tumor. Lymphocytes are a type of white blood cells that play a key role in the function of the immune system. In their study, the Washington State University researchers focused specifically on a type of lymphocytes called CD4-positive helper T-cells.
Other current hurdles in cancer immunotherapy include:
- Unpredictability in the efficacy of the treatment
- Tumor heterogeneity often impedes efficacy
- Development of resistance to treatment
- Difficulty identifying significant biomarkers
- A lack of predictive biomarkers
- Immunotherapy-specific clinical designs are needed
What do CD4 and CD8 T-cells do in the immune system?
T-cells are categorized in the lymphocyte blood cell class and work in the body’s lymphatic system. While most previous research and many current immunotherapies have focused on a type of killer white blood cell called CD8-positive T-cells, this study analyzed CD4-positive helper T-cells.
CD4 T-cells stimulate other immune system cells in an effort to coordinate the immune system response to fight against infection. These other immune cells include CD8 cells, as well as macrophages and B lymphocytes (B-cells).
The immune system also has two types of killer blood cells: CD8-positive T-cells and natural killer cells. Both of these cells attack cancer cells and virally infected cells. Natural killer cells move throughout the body and are the immune system’s first defense mechanism, but they are unable to identify specific types of antigens. CD8-positive T-cells kick in after the natural killer cells and are better able to recognize specific antigens.
CD8-positive T-cells are used in several current immunotherapies and have been the subject of extensive research, but scientists know relatively little about how to activate the antitumor function of natural killer cells.
Despite the prevalence of CD8-focused immunotherapies, less than 20% of patients respond to them. Lead author Hui Zhang believes that CD4-positive helper cells could be used in an initiating role to make CD8-positive immunotherapies more effective.
Testing CD4-positive T-cells on mice samples
The team of researchers at Washington State University made their discovery during CD4-positive T-cell experiments on mice samples. They found evidence that a subset of CD4-positive T-cells called tissue-resident memory T-cells could play a vital role in activating the natural killer cell defense system.
The experiments showed that these cells were effective against breast cancer tumors and melanoma. According to Zhang, these cells were key in the initiation of the antitumor immune response.
The tissue-resident memory T-cells worked with the natural killer cells to kill tumor cells and also controlled tumor progression, along with improving the infiltration of other white blood cells into the tumor.
Future research based on these findings
The Washington State University researchers plan to build off of these findings in future studies. Specifically, they plan to study the exact cellular and molecular mechanisms involved in this type of anti-tumor immunity.
These mechanisms will first be investigated in mice samples to develop an effective cancer immunotherapy. If successful at this stage, the researchers will test the immunotherapy on human subjects in clinical trials.
While a great deal of research still needs to be conducted, there is reason to be optimistic that these results could be used to craft a new and more effective form of cancer immunotherapy. These researchers may have discovered a solution to one of the most perplexing hurdles in current immunotherapy research.