Researchers at the Institute of Cancer Research in London have developed a groundbreaking light-activated therapy that could be used to better detect and treat an aggressive form of brain cancer, according to the findings of a recent study. Dubbed “photoimmunotherapy”, this innovative treatment uses a fluorescent dye that contains a compound that targets cancer, which can be used to strengthen the body’s immune response.
Oncology experts are extremely optimistic about the implications of this new study, with some positing that photoimmunotherapy could become the fifth major cancer treatment—following surgery, chemotherapy, radiation, and immunotherapy. Here is a deeper look at these findings and how they might be used to help those struggling with aggressive brain cancer.
How Does Photoimmunotherapy Work?
Photoimmunotherapy is a light-based cancer therapy that causes cancer cells to glow in the dark. This allows surgeons to remove a larger portion of the tumors compared to the current standard surgery techniques. Within minutes of the end of the surgery, the photoimmunotherapy compound destroys all remaining cancer cells.
Previous studies have focused on a form of photoimmunotherapy called near-infrared (NIR-PIT), which uses infrared light to trigger the immune system to rapidly and selectively kill cancer cells. To be more specific, NIR-PIT uses an antibody-photoabsorber conjugate that binds to cancer cells. The near-infrared light activates the cells and causes them to grow and eventually explode, which kills the cancer cells.
The Institute of Cancer Research study was based on trials of a new type of photoimmunotherapy that uses synthetic molecules called affibodies, which are proteins engineered to bind to specific targets with high accuracy. The affibodies were bonded with a fluorescent molecule called IR700, which is used to identify tumor masses during surgery.
Challenges in Treating Glioblastoma
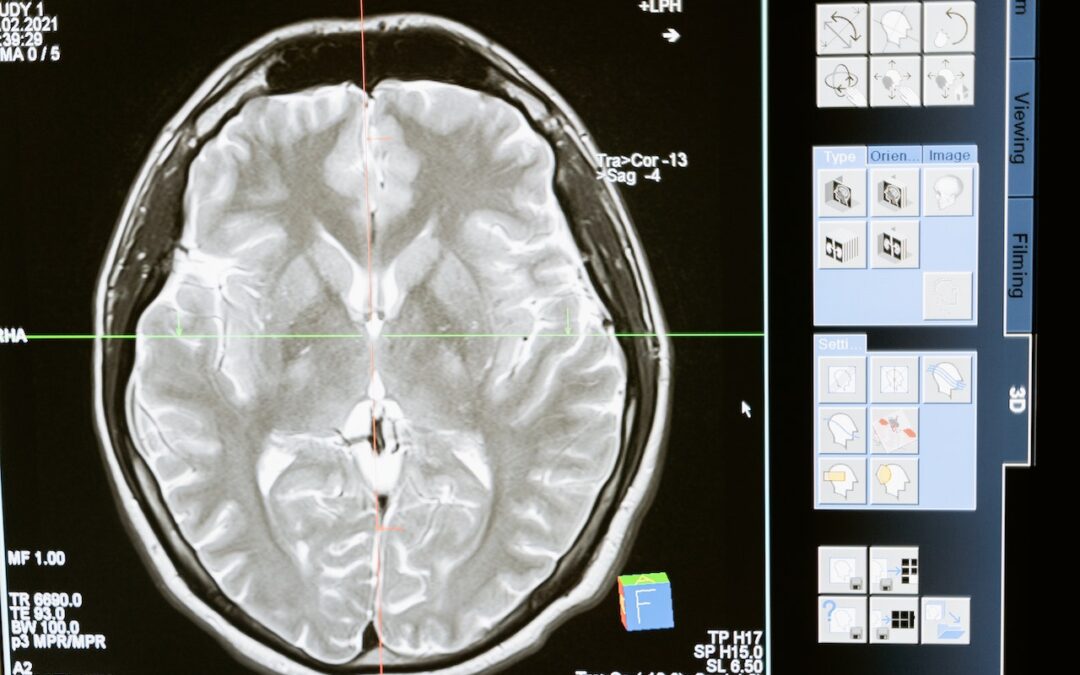
The ICR trials investigated whether this new form of photoimmunotherapy could be used to treat a form of brain cancer called glioblastoma, one of the most aggressive and difficult-to-treat variations of the disease. Currently, many surgeons use a method called fluorescence-guided surgery to treat glioblastoma and other forms of brain cancer. This method uses dyes to highlight the tumor mass that needs to be removed during surgery.
Glioblastoma is difficult to treat because these tumors grow in sensitive areas of the brain, like the motor cortex. Following surgery, glioblastoma patients often have residual tumor cells that can be extremely difficult to remove. This leads to a high recurrence rate after surgery.
Methodology and Findings of Mice Study
Researchers from ICR and the Medical University of Silesia, Poland tested the affibody conjugate (scientific name ZEGFR:03115-IR700) on mice with glioblastoma. They observed that the cancer-targeting compound became fluorescent in the brain tumors during surgery, only about one hour after the compound had been administered.
The near-infrared light was aimed at the tumor cells, which triggered the anti-tumor effects of the compound and killed cancer cells. The mice treated with the compound showed significant evidence of tumor cell death compared to untreated mice.
The photoimmunotherapy also activated immune responses in the body that could prepare the immune system to target cancer cells. This suggests that photoimmunotherapy could be used to prevent glioblastoma cells from returning following surgery.
Potential Applications of These Findings
Cancer survival rates have drastically improved due to advancements in surgery, chemotherapy, radiotherapy, and immunotherapy. However, the efficacy of these treatment methods varies depending on the type and severity of the patient’s cancer. Those who have glioblastoma and certain other cancers that occur near vital organs are often at a high risk of complications when undergoing surgery.
Photoimmunotherapy could provide a solution to this issue by allowing surgeons to target and eliminate tumors without risking harm to these vital organs. In addition, this form of treatment could be used to target cancer cells that are unremovable during surgery.
The ICR researchers are hopeful that their findings could be adapted for the treatment of other types of cancer. The next steps will involve conducting clinical trials with human glioblastoma patients. If the success of this treatment is replicated in those trials, researchers will likely begin exploring whether this form of photoimmunotherapy could be similarly effective in treating other cancers.
Further Research
The ICR researchers believe that additional work is needed before the full potential of photoimmunotherapy as a glioblastoma treatment, especially concerning local and systemic immune responses and interactions with post-surgical treatments. Further research is also needed for the practical applications of administering this treatment, including evaluations of light intensity, light delivery protocols, and radiation doses.
Despite these remaining challenges, the researchers believe that the results of this study are extremely promising. Photoimmunotherapy seems to have exciting potential as a novel treatment for this form of brain cancer, which is notoriously difficult to treat.